Why did we do the study?
The implementation of Health TAPESTRY in six communities across the province involved a nine-partner community-academic partnership (CAP): one academic partner, two non-profit organizations, and six primary care practices. There are many barriers, facilitators, and considerations that occur when forming and engaging in this kind of partnership, many of which are well described in the literature. However, little is known about what topics CAPs actually focus on and how those discussions impact implementation at the local sites, which is what we wanted to explore in this study.
What did we do?
We analyzed 128 meeting minutes from CAP members as well as 278 provider and client surveys about what worked best and worst in the program. We then brought the analysis back to some of the key informants to further understand our findings.
What did we find?
The CAP partners’ discussions focused on a wide range of topics, many of which were not identified by providers and clients as substantial positives or negatives of the program. The CAP partners mostly discussed topics at a higher level that did not directly relate to on the ground implementation. Their key categories of discussion were:
- Primary care sites
- Volunteer coordination
- Volunteer experience
- Internal and external connections
- Sustainability and scalability
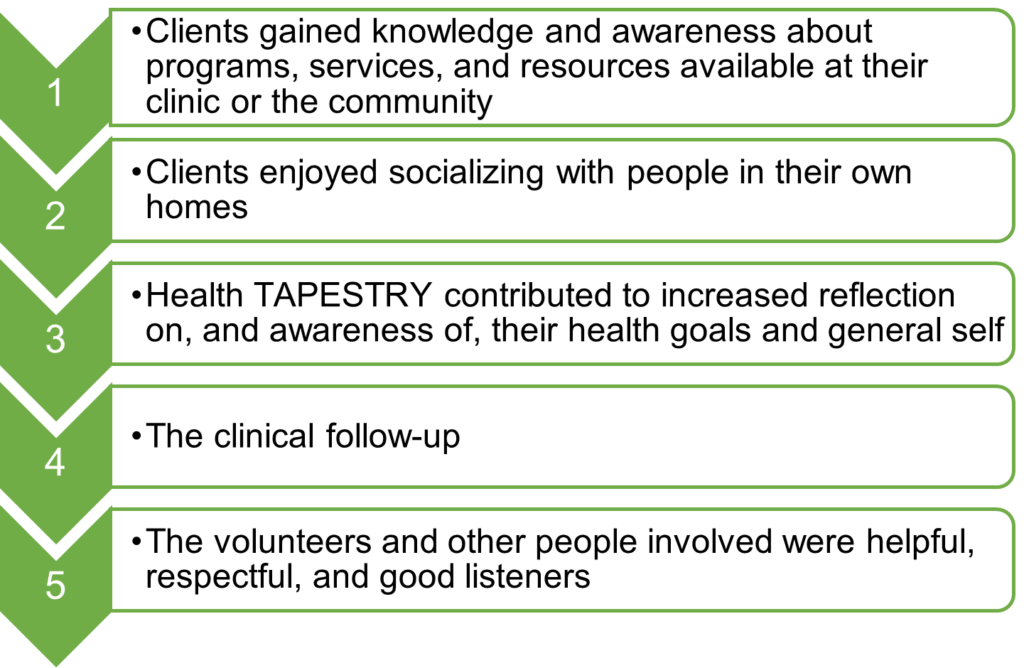
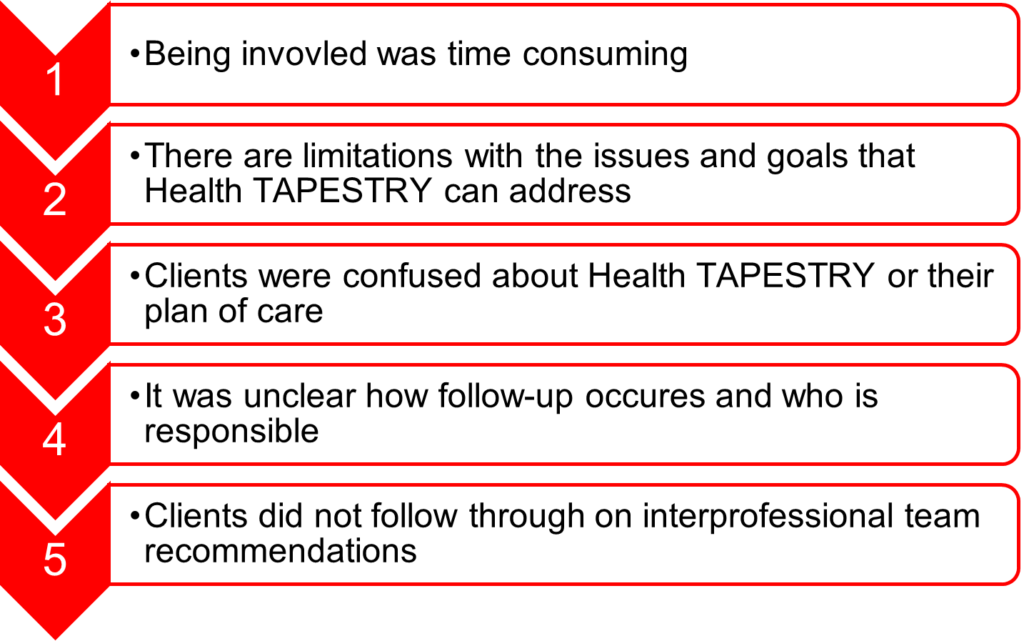
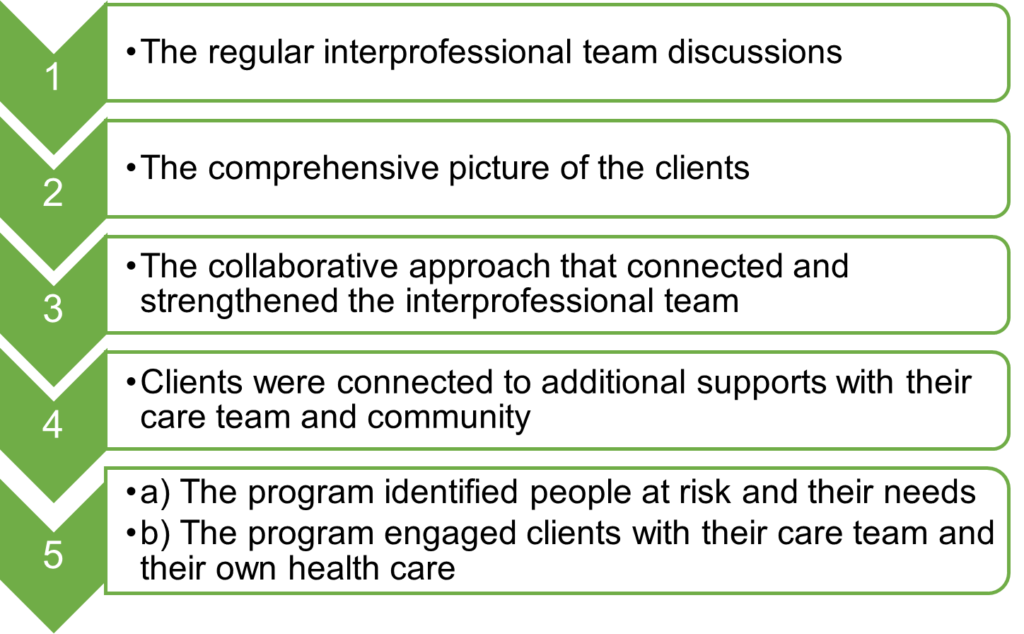
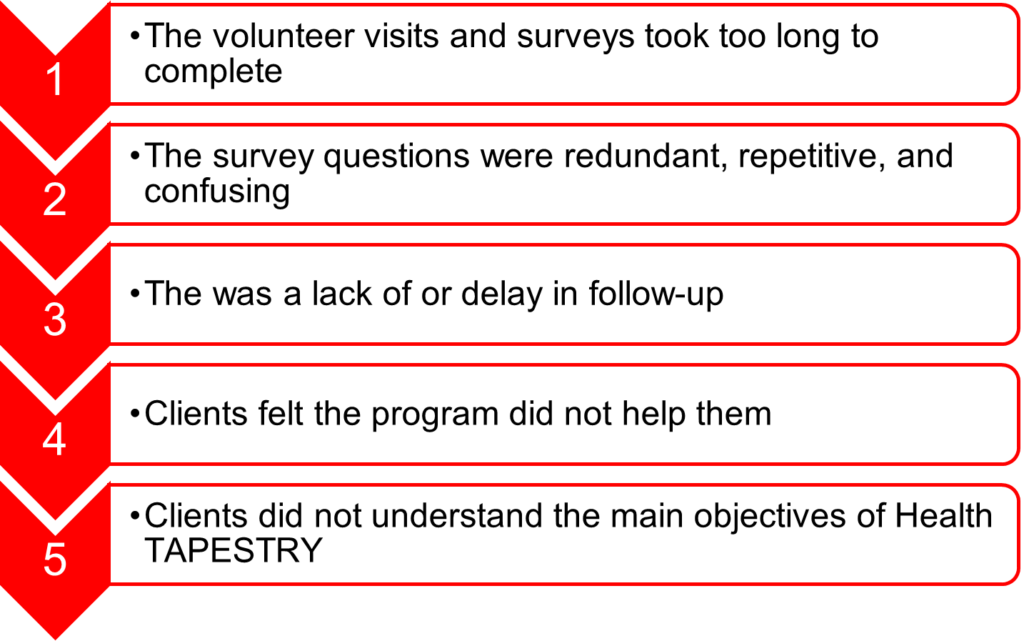
The things that clients and the providers noted that worked the best and worst related more to “on the ground” implementation. These were not always relevant for the CAP partners at the planner/decision-maker level to discuss. Some of the elements were also unrelated to the program itself (e.g., clients liking the volunteers themselves), but rather a product of how and by whom the program was administered.
What do our findings mean?
One important learning is about who had “voice” at the planner/decision-maker level. As described above, many of the topics discussed in meeting minutes were not identified by clients or providers, and vice versa. This may indicate their different roles and needs, but may also indicate a gap.
We also identified three phases in our work that could serve as a guide for other CAPs:
- Phase 1: Recruitment, financial support, and data ownership
- Phase 2: Considerations for modifications and adaptations
- Phase 3: Active input and reflection
What the Clients Liked and Didn’t Like
What the Interprofessional Team Members Liked Best and Didn’t Like
The full article can be found here: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09617-y

